Case 1:
Our first “Eyes of the Month” case study follows an older patient who experienced sudden onset vision blurriness in only one eye, along with depth perception issues.
Patient Visit:
An 80-year-old male from North Queensland was referred to Queensland Eye and Retina Specialists with a three-day history of sudden onset blurred vision in the left eye. He first noticed blurred vision after waking from an afternoon nap. He had also been having difficulty with depth perception (he had missed the cup when pouring a drink and cut his finger whilst cooking).
Past ocular history was consistent with his age, having had uncomplicated bilateral cataract surgery in his early 60s. There was no history of head trauma. There was no significant past medical history or family ocular history.
Ocular exam revealed the following:
Unaided Visual Acuity:
RE: 6/6= LE: Count Fingers (CF)
Best Corrected Visual Acuity:
RE: -0.25/-0.75 x 80 (6/4.5-) LE: +9.50 (6/7.5)
Intraocular Pressure (iCare):
RE: 15mmHg LE: 10mmHg
Pupils: EA, DCN No RAPD
External examination with slit lamp was within normal limits.
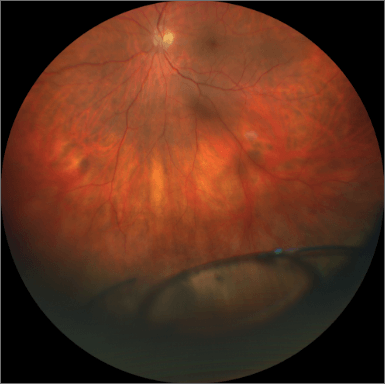
Dilated fundus examination revealed a total out-of-the-bag dislocation of a 3-piece IOL in the inferior vitreous chamber (Fig1). All other posterior structures were unremarkable.
Diagnosis and Discussion
Diagnosis:
LE dislocated 3-piece IOL.
Differential diagnoses:
Nil
Discussion:
As a result of sustained increasing life expectancy, more and more people are undergoing cataract surgery. IOL dislocation is a serious potential complication following cataract surgery, with a reported world-wide incidence rate of between 0.05% to 3%. As such it is important that optometrists are able to identify and appropriately manage this complication.
IOL decentration, dislocation and subluxation are commonly interchanged these days, however describe slightly different presentations. Decentration usually refers to movement of the lens out of alignment without loss of zonular integrity. Subluxation involves partial loss of zonular stability and dislocation is due to total loss (Fig2).
In most cases IOL dislocation is related to the integrity of the capsular bag and zonules. It is therefore important to be aware of predisposing conditions, including; previous vitreoretinal surgery, aging, axial myopia, uveitis, trauma, mature cataract and connective tissue disorders (ie PXF, Marfan’s syndrome, Ehler’s Danlos Syndrome etc).
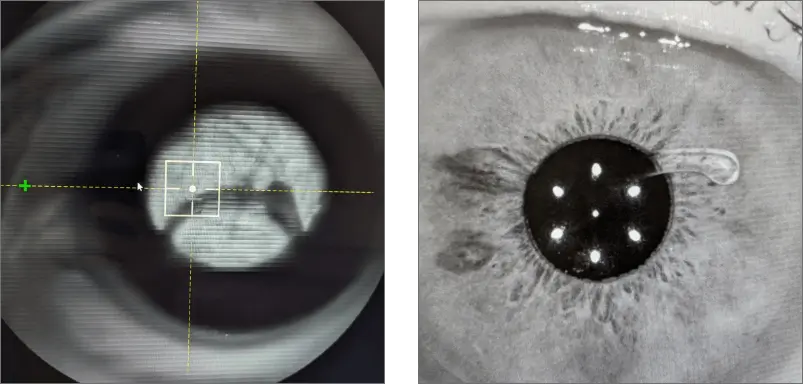
Figure 2: Different ways in which lenses can decentre or dislocate. Some lenses may dislocate into the anterior chamber.
Treatment:
In patients with minimal decentration or subluxation and thus well-preserved visual function, close observation may be an appropriate initial treatment. If opting for this management option, patients need to be educated of the potential for intermittent angle-closure glaucoma and its associated symptoms (pain, blurred vision, nausea, increased eye redness).
The most common treatment option, and the one chosen for the above case, is an IOL exchange. For this procedure the original IOL is retrieved and a secondary IOL is implanted. The type of secondary IOL used is dependent on the integrity of the capsular bag and surrounding structures. Options include placing the lens in the sulcus, anterior chamber or scleral fixation.
The above patient had an anterior chamber intraocular lens (ACIOL) implanted due to the absence of adequate capsular support (Fig 3). Modern ACIOLs have been modified to reduce complication risks, by incorporating footplates (to reduce angle contact) and anterior vault (to decrease likelihood of iris chafe). As the lens cannot be folded, a larger incision is required, which will temporarily induce a significant amount of astigmatism. A peripheral iridotomy is also necessary to prevent pupillary block. As this lens is located anteriorly in the eye compared to a regular intracapsular IOL, they require less overall refractive power.
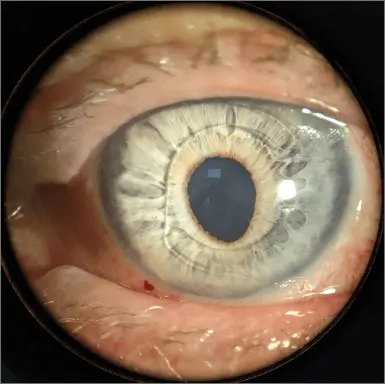
Figure 3: The anterior chamber IOL with its haptics extending to the angle. The peripheral iridotomy can be seen at 4 o’clock on the iris.
One-month Post Operative Results:
Unaided Acuity:
LE 6/18
Best Corrected Visual Acuity:
LE +2.00/-2.00 x 7 (6/7.5)
With a few more weeks healing it is likely some of this astigmatism will resolve as the suture (which are superior) dissolve and the cornea relaxes. As Toric ACIOLs are not available, patients are always counselled on the fact that they may require glasses post operatively.
Have any questions about patient eye care?
Contact Queensland Eye & Retina Specialists for more information.
Queensland Eye & Retina Specialists
accepts referrals via email, Oculo, Medical Objects and fax.