Case 2:
To celebrate World Glaucoma Week, our March “Eyes of the Month” case study follows an older gentleman who was urgently seen for raised intraocular pressure that resulted in glaucoma.
Patient Visit:
A 66-year-old gentleman was urgently referred to Queensland Eye and Retina Specialists on a Wednesday afternoon at 4:30pm for raised intraocular pressure. He had been to see his local optometrist to get new glasses as he had broken his previous pair. At the optometrist he noted that his vision in his right eye had been fluctuating in and out for the past 2-3 weeks along with some slight flashes of light.
Previous ocular and medical history were unremarkable for his age, although he had seen an ophthalmologist in the past, but he was not sure why. There was a family history of retinal detachment, with his brother having surgical repair for bilateral detachments.
Ocular exam revealed the following:
Best Corrected Visual Acuity:
RE: +3.75/-1.00 x 90 (6/6) LE: +4.50/-1.75 x 95 (6/6=)
Intraocular Pressure (iCare):
RE: 45mmHg LE: 14mmHg
Pupils: EA, DCN No RAPD
External examination with slit lamp revealed a moderately injected conjunctiva on the RE. Both corneas appeared clear. Both eyes demonstrated shallow anterior angles. Anterior OCT imaging (Fig1, 2) revealed closed angles nasally in the RE and narrow angles in all other quadrants for both eyes. Gonioscopy confirmed the findings of angle closure in three quadrants in the RE and near closure in the LE.
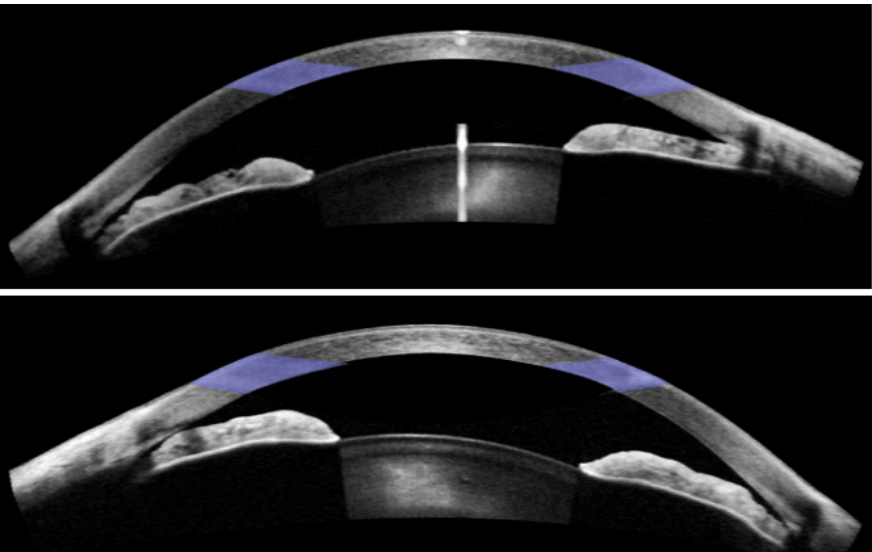
Figure 1: Anterior chamber OCT imaging for RE (top) and LE (bottom).
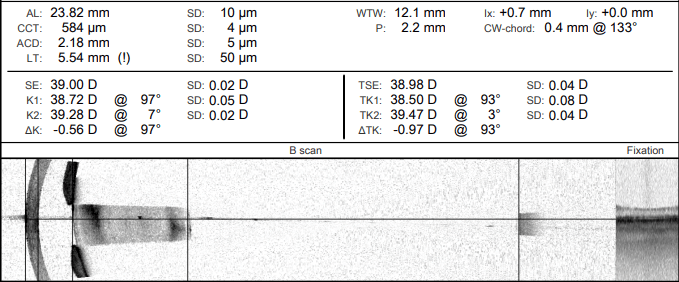
Figure 2: Biometry scans of the RE, showing increased lens thickness and narrow anterior chamber depth.
Diagnosis and Discussion
Diagnosis:
RE angle closure glaucoma secondary to phacomorphic cataract
Differential diagnoses:
Primary angle closure glaucoma
Discussion:
Angle closure glaucoma is a relatively common cause of blindness, with a particularly high prevalence in some populations. There are a number of risk factors for angle closure, including: increasing hyperopia, family history of angle closure, advancing age, female gender, Asian or Inuit descent, and short axial length.
There are two forms with distinct pathophysiology, primary angle closure, and secondary angle closure. Primary angle closure is most commonly caused by relative pupillary block, where aqueous flow from posterior to anterior is impeded, causing an increased posterior pressure gradient. This in turn causes bowing of the iris forward, causing the iris to cover and therefore occlude the trabecular meshwork. Secondary angle closure can occur as a result of a number of other eye diseases, either pushing the iris forward from behind or pulling the iris into contact with the trabecular meshwork. Conditions which can cause secondary angle closure include anterior or posterior synechiae, intumescent cataract, ectopia lentis, aqueous misdirection, ciliary body, or choroidal swelling.
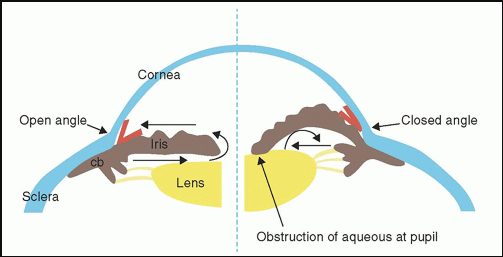
Figure 3: Normal unimpeded aqueous flow on the left versus impeded flow due to iridolenticular contact on the right. Image courtesy of Dr. Sandra Fernando Sieminski.
Treatment:
As the adage goes, “prevention is better than cure”, and this is definitely apposite in the case of angle closure glaucoma. Optometrists play a vital role in appropriate screening and referral of patients who may be primary angle closure suspects (PACS). Measurement of anterior chamber angles can be achieved using the Van Herick technique on a slit lamp biomicroscope. If a patient is thought to have narrow angles, further investigation with gonioscopy is warranted. At risk patients can then be referred to a glaucoma specialist for consideration of prophylactic peripheral iridotomy (PI).
In diagnosed cases of acute angle glaucoma, treatment may include medical therapy, surgery, or both. Initially the aim should be lowering IOP as much as possible to reduce pain and clear corneal oedema. Both topical and systemic medications can be used, of course bearing in mind any contraindications. Laser PI can be used to create another channel for aqueous to flow, bypassing any pupillary block and equalising pressure between the posterior and anterior chamber (Fig.4). In cases of secondary angle closure glaucoma, it is necessary to further address underlying pathology.
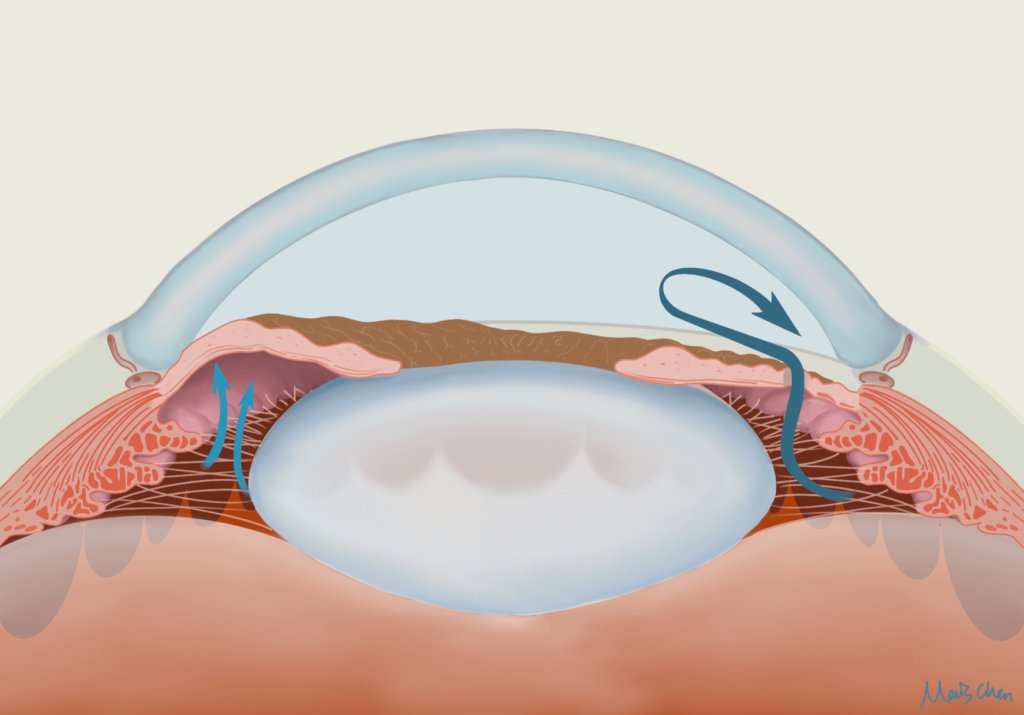
Figure 4: Patent Laser Peripheral Iridotomy allowing aqueous to bypass pupil block and flow from posterior to anterior chamber.
As the gentleman discussed earlier was demonstrating symptoms of acute angle closure, immediate treatment was required. The patient was not nauseous, so 500mg oral acetazolamide (a carbonic anhydrase inhibitor) was administered. It was also decided to undergo bilateral laser peripheral iridotomy to aid in aqueous outflow, following treatment pressure reduced from 45mmHg to 24mmHg in the RE. Given the underlying cause for the angle closure was intumescent cataract, the patient was scheduled for bilateral cataract surgery (two weeks apart) as soon as possible. In order to control IOP until cataract surgery could be completed, the patient was started on oral Diamox three times a day (for 1 day) and topical GanForte PF at night in both eyes.
Two-month Post Operative Results:
Unaided Visual Acuity:
RE: 6/6= LE: 6/6=
Intraocular Pressure (iCare):
RE: 14mmHg LE: 15mmHg
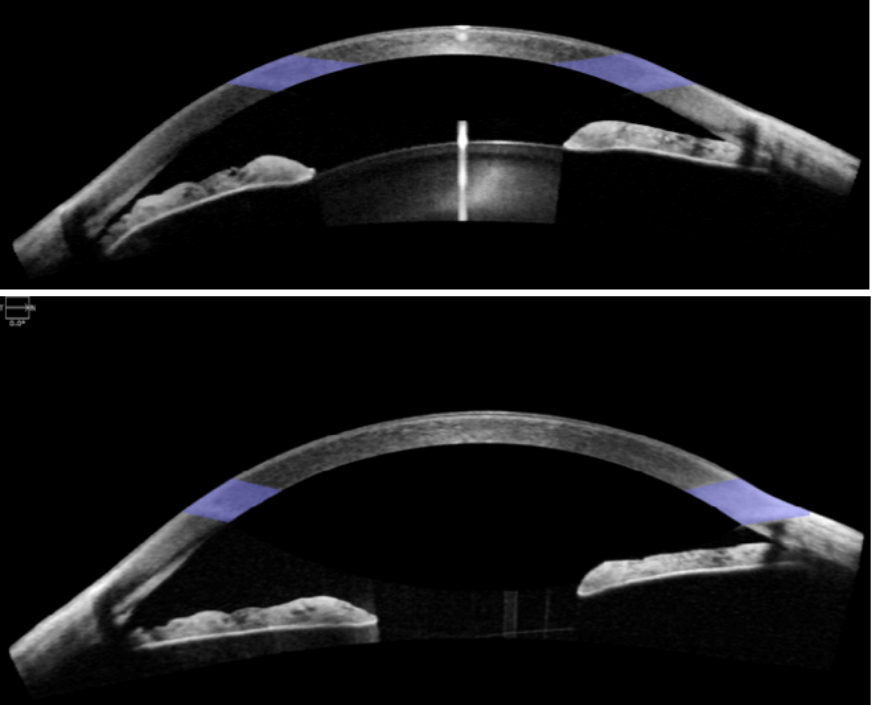
Figure 5: Anterior chamber OCT of the RE before (top) and after (bottom) cataract surgery, demonstrating the now open anterior angle.
Have any questions about patient eye care?
Contact Queensland Eye & Retina Specialists for more information.
Queensland Eye & Retina Specialists
accepts referrals via email, Oculo, Medical Objects and fax.