Case 3:
Patient Visit:
A 55-year-old female attended Queensland Eye and Retina Specialists at the request of her treating ophthalmologist, for assessment of her left macula. She did not have any particular concerns and was asymptomatic.
Past ocular history included bilateral cataract surgery 4 months prior and a very mild amount of post-operative cystoid macular oedema (CMO) in the LE. She had a family history of early cataracts (her father underwent cataract surgery in his early 50s), and a strong history of diabetes in the family, particularly on her mother’s side. The patient was also a type 2 diabetic (onset 10 years ago), with recent HbA1c of 6.5% and had medically controlled mild hypertension and hyperlipidemia.
Ocular exam revealed the following:
Unaided Visual Acuity:
RE: 6/4.5 LE: 6/7.5-
Intraocular Pressure (iCare):
RE: 11mmHg LE: 10mmHg
Pupils: EA, DCN No RAPD
External examination with slit lamp was within normal limits.
Internal examination revealed well positioned intraocular lenses in both eyes. OCT and Optos imaging for the LE can be seen below.
As can be seen in Figure 1, there is vitreomacular traction (VMT) localized to the area nasal to the fovea. There is some loss of the foveal architecture and external-limiting membrane (ELM) and retinal pigment epithelium (RPE) changes at the fovea. The Optos (Figure 2) image shows fibrotic changes, regressed NVE and scattered dot haemorrhages, the right eye has a relatively featureless fundus appearance.
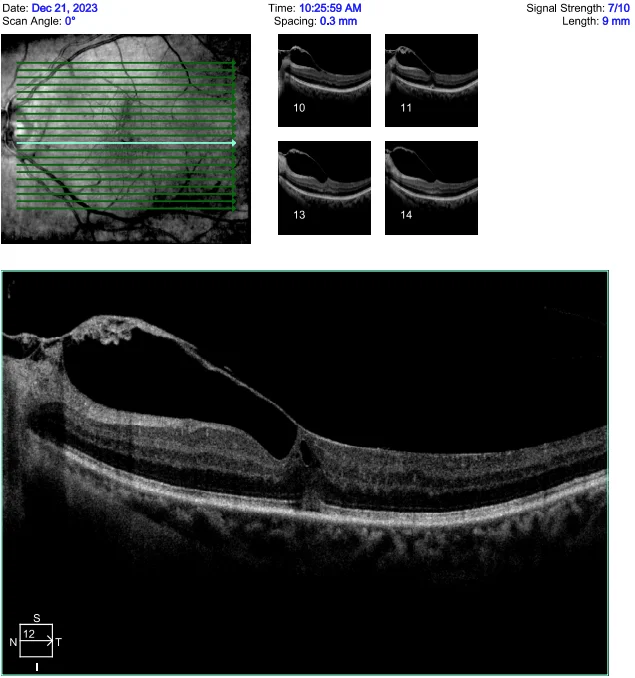
Figure 1: 21-Line high-definition macular scan of the LE, demonstrating vitreomacular traction.

Figure 2: Optos image showing fibrotic changes, regressed NVE and scattered dot haemorrhages.
Diagnosis and Discussion
Diagnosis:
Left eye vitreomacular traction (VMT)
Bilateral partially regressed proliferative diabetic retinopathy (PDR)
Discussion:
The case discussed above is a good example of why we should do a comprehensive eye examination to ensure we do not miss any less obvious eye disease, as it is not uncommon for people to have more than one ocular pathology at a time. Indeed, in this case, as the patient has no symptoms of VMT (metamorphopsia, central scotoma etc.) and it has been stable for some time, the more pressing issue is management of the diabetic retinopathy.
Diabetes is a chronic health condition which can lead to serious damage to the heart, kidneys, blood vessels, nerves and eyes. Diabetic eye disease can be classified into two separate types; non-proliferative and proliferative. Signs of non-proliferative retinopathy can include microaneurysms, dot-blot hemorrhages, venous beading and intraretinal microvascular anomalies (IRMA). NPDR can be further classified as mild, moderate or severe depending on how widespread the previous vascular changes are. If there are any new vessels present, this is referred to as proliferative diabetic retinopathy.
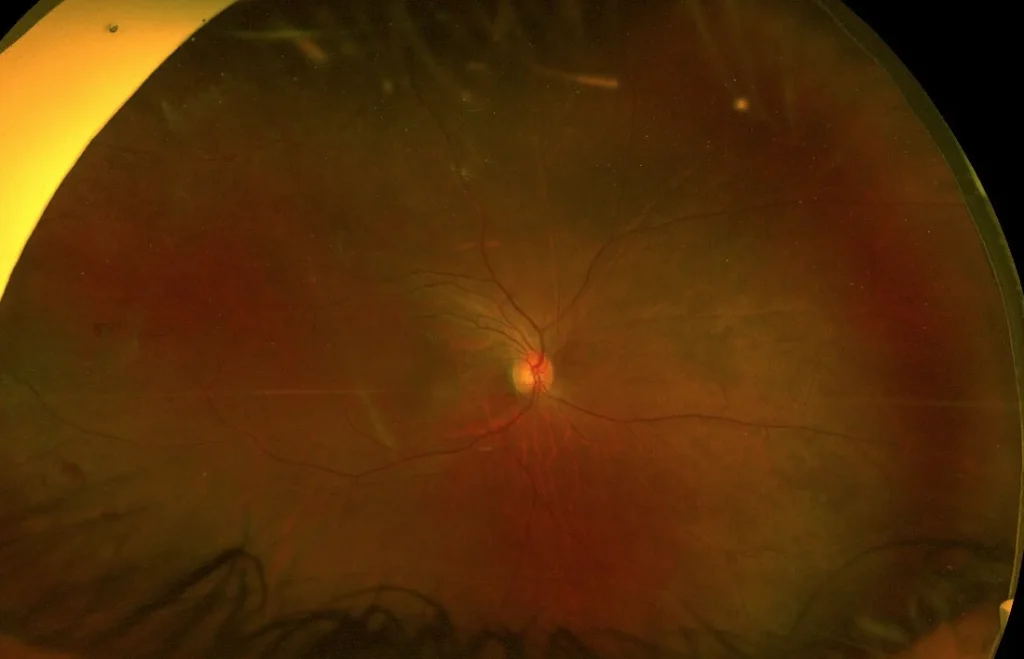
Figure 3: A relatively featureless Optos image of the patients’ right eye. Only a small number of microaneurysms can be seen.
Under dilated examination an area of NVE in the supero-temporal retina can also be seen in the right eye. In this case, given the featureless fundus in conjunction with NVE in both eyes a fundus fluorescein angiogram (FFA) is warranted to fully investigate the extent of diabetic changes and develop an appropriate treatment plan.
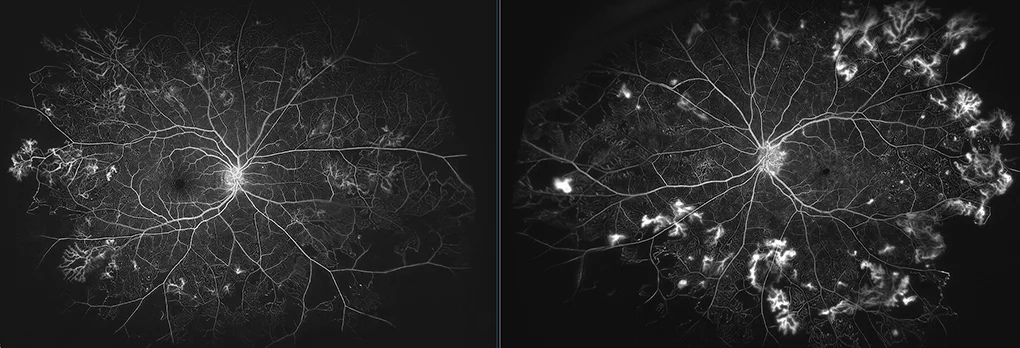
Figure 4: FFA demonstrating florid NVE and ischemia
After undergoing fluorescein angiography there are significant proliferative diabetic changes which may otherwise have been missed. Both eyes demonstrate florid NVE with vascular leak, as well as multiple areas of peripheral retinal ischemia. Untreated, these NVE may lead to further complications, including diabetic macula edema, further neovascularization or tractional retinal detachment.
Early detection of retinopathy is critical and can help prevent up to 98% of severe visual impairment. Patients with diabetes should undergo a comprehensive dilated eye exam annually, to check for any signs of diabetic retinopathy.
Treatment:
Both eye conditions will need concurrent management plans. In regards to the left vitreomacular traction, as the patient is asymptomatic, it is appropriate to follow this closely (both with longitudinal OCT scanning and self-monitoring with an Amsler grid). If change is noticed, surgical intervention with vitrectomy and epiretinal membrane peeling may be warranted.
Given the extent of proliferative diabetic changes, the patient requires bilateral panretinal photocoagulation (PRP). This treatment delivers laser burns to the peripheral retina, with the aim of reducing VEGF release and promoting regression of neovascularization. This treatment is not curative, but rather designed to lessen the future risk of vitreous haemorrhage and tractional detachment.
1 Month Post PRP Treatment:
Unaided Visual Acuity:
RE: 6/6 LE: 6/7.5
At review one-month after bilateral PRP there was evidence that the proliferative retinopathy had become quiescent. There was excellent uptake of the laser treatment, as can be seen in Figure 4 below. There was no progression of the VMT in the LE
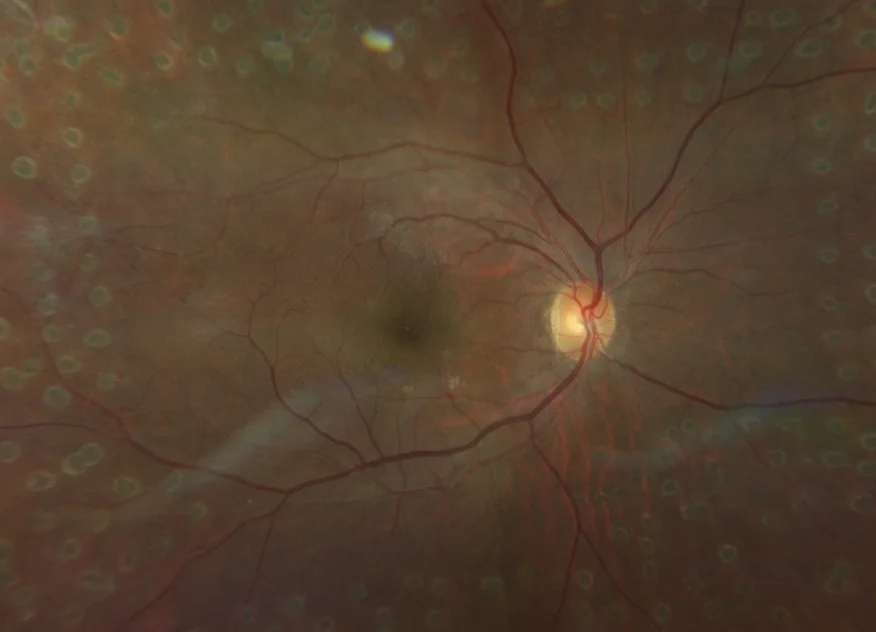

Figure 5: Characteristic appearance of laser burns in the peripheral retina following PRP.
Have any questions about patient eye care?
Contact Queensland Eye & Retina Specialists for more information.
Queensland Eye & Retina Specialists
accepts referrals via email, Oculo, Medical Objects and fax.