Case 8:
This month’s Eyes of the Month involves an elderly man who visited QERS after experiencing progressive difficulty reading over a 6-month period, which resulted in a diagnosis of ARMD.
Patient Visit:
A 77-year-old male attended Queensland Eye and Retina Specialists after noticing progressive difficulty with reading vision over the past 6 months. He was not particularly bothered by the changes, and had visited his optometrist with the intent of upgrading his reading glasses. The patient was unaware if the changes were specific to one eye.
Past ocular history included surgical excision of conjunctival telangiectasia on the left eye, which thankfully turned out to be benign on histological examination. Other than taking candesartan for hypertension he was in excellent general health and is an ex-smoker. Family ocular history included age-related macular degeneration.
Ocular exam revealed the following:
Best Corrected Visual Acuity:
RE: +1.00/-0.50 x 90 (6/7.5) LE: +1.00/-1.00 x 90 (6/18)
Intraocular Pressure (iCare):
RE: 12mmHg LE: 13mmHg
Pupils: EA, DCN No RAPD

External examination with slit lamp biomicroscope was unremarkable, other than age-appropriate cataracts in both eyes.
Dilated fundus examination revealed pigmentary changes at both the macula and peripheral retina of the left eye (Fig1). Symmetrical cupping of 0.8 was evident in both right and left eyes.

Figure 1: Fundus photography of the LE demonstrating pigmentary changes at the macula and peripheral drusen.
Optical coherence tomography (OCT) of the left posterior pole revealed disorganisation of the retinal pigment epithelium (RPE), serous pigment epithelial detachment (PED) and thickening of the foveal architecture (Fig2). OCT angiography also provides evidence of erythrocyte flow in the outer-retinal complex, which is usually avascular, suggesting the presence of an active choroidal neovascular membrane (CNVM) (Fig3).

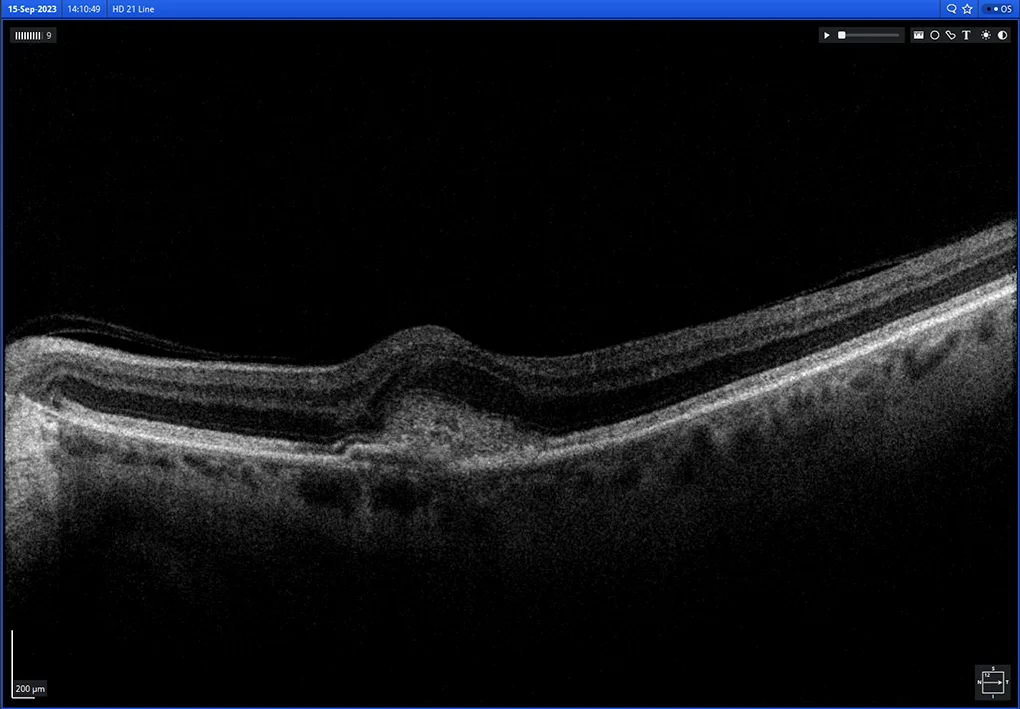
Figure 2: OCT imaging of the macular region of the left eye, demonstrating serous PED (above) and RPE disruption (below).

Figure 3: OCT-A scanning of the LE macular region, revealing active CNVM (as demonstrated by a hyperfluorescent network of vessels) in the normally avascular outer retinal complex.
Diagnosis and Discussion
Diagnosis:
LE exudative age-related macular degeneration (ARMD)
Differential diagnosis:
- Choroidal rupture
- Pathologic myopia
- Angioid streak associated CNVM
- Central serous chorioretinopathy
Discussion:
ARMD is the most common macular disease in Australia, accounting for half of all blindness and severe vision loss. The prevalence of ARMD is estimated at around 1.5%, a figure which sharply increases over the age of 75.
The symptoms of ARMD include loss of central visual acuity, metamorphopsia, central scotoma and trouble reading.
Natural aging changes and the pathophysiological changes associated with ARMD can be difficult to distinguish. It is likely that cumulative oxidative injury to components of the retina underpin both normal and abnormal processes. Importantly, small, hard drusen commonly seen with age are composed of distinctly different materials to the large, soft, confluent drusen classically seen in ARMD.
Treatment:
The medical therapies and lifestyle alterations to help prevent and treat ARMD are well researched and well known. The advent of OCT technology and anti-VEGF medications, such as Avastin, Eylea, Lucentis, Beovu and Vabysmo, have revolutionised treatment and outcomes for patients with exudative-ARMD.
However, once an optometrist refers a patient with suspected ARMD to an ophthalmologist, they may be unaware of the particular protocol for treatment. RANZCO have robust, research-based guidelines for treatment protocols for ARMD. In general, new patients with confirmed ARMD should undergo a loading dose of 3 intravitreal injections, 4-6 weeks apart, most commonly with Eylea or Lucentis. At each visit BCVA and OCT should be completed to monitor progression. If adequate response is achieved with the loading dose, a “treat-and-extend” protocol can be adopted, whereby the interval between injections is increased by two weeks (e.g., 6 weeks, 8 weeks, 10 weeks, 12 weeks). If inadequate response is achieved after the loading dose, the ophthalmologist may decide to use the alternate medication (i.e. Lucentis to Eylea or vice versa) or change to Vabysmo (faricimab). This drug is a monoclonal antibody which targets both vascular endothelial growth factor and angiopoietin 2. The risks of this medication, unlike Eylea and Lucentis, can include vasculitis (approximately 1 in 60,000) and therefore is primarily used as a second line agent. If this medication is successful the “treat-and-extend” protocol can again be used.
In most cases treatment for exudative-ARMD is lifelong, which can cause a significant financial burden for patients. It is important they are aware of this before commencing any treatment. For some, if treatment with all medications has been unsuccessful, or there has been stability without treatment for 12 months, they may be discharged for follow-up to their local optometrist.
Follow-Up:
At the initial visit a diagnosis of exudative-ARMD was reached and the decision to begin intravitreal anti-VEGF injections (with Eylea) was made. An initial loading dose of 3 injections spaced out monthly administered. The OCT scans for each injection visit demonstrate complete resolution of the serous fluid and overall reduction in macular thickness (Fig 4).
The reduction in fluid and macular thickness was accompanied by an improvement in visual acuity.
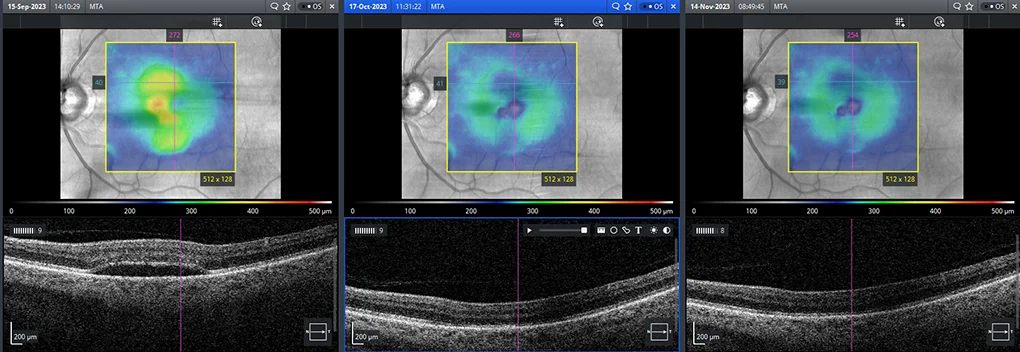
Figure 4: A series of macular thickness OCT images taken at each of the 3 injection visits (left most image is baseline). After the first injection there is complete resolution of serous PED and improved macular thickness.
Best Corrected Visual Acuity:
RE: +1.00/-0.50 x 90 (6/7.5) LE: +1.50/-1.00 x 90 (6/9++)
The decision was made to “treat-and-extend”, with another series of injections, spaced 6 weeks, 8 weeks, 10 weeks and 12 weeks. The longest interval ophthalmologists will generally leave between injections is 12 weeks. Unfortunately, at the 12-week interval there was recurrence of subretinal fluid (Fig 5), and the decision was made to continue injections at 10-week intervals.

Figure 5: Recurrence of subretinal fluid on macular OCT.
Is your patient experiencing difficulty readding?
Send them to Queensland Eye and Retina Specialists for personalised care and treatment.