Case 10:
This month, our Eyes of the Month blog follows an elderly woman who was referred to QERS after an onset of flashes, floaters and a shadow in her nasal visual field. Examination eventually led to a diagnosis of macula-ON rhegmatogenous retinal detachment (RRD).
Patient Visit:
A 61-year-old female from central Queensland was referred to Queensland Eye and Retina Specialists following a three-day history of sudden onset flashes, floaters and a shadow in her nasal visual field of the right eye. The shadow had been progressing slowly over the previous three days.
Her past ocular history was unremarkable, with no previous surgery or significant injuries or infections. She was not diabetic and had no other known comorbidities. Family ocular history was also unremarkable.
Ocular exam revealed the following:
Unaided Visual Acuity:
RE: 6/18= LE: 6/12=
Best Corrected Visual Acuity:
RE: +1.25 (6/9=) LE:+1.00 (6/12=)
Intraocular Pressure (iCare):
RE: 9mmHg LE: 11mmHg
Pupils: EA, DCN No RAPD
External examination with slit lamp was within normal limits.

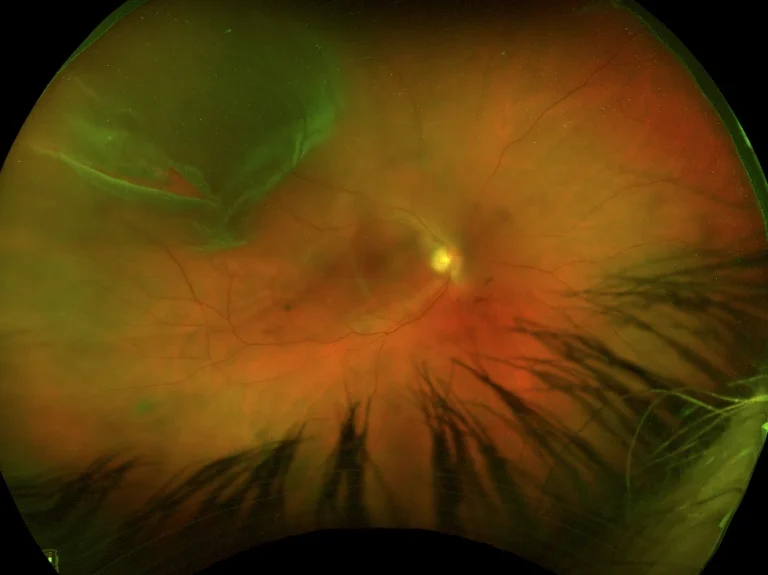
Figure 1: Optos Ultrawide field imaging of the RE, revealing a superior retinal tear and associated detachment.
Internal examination through dilated pupils revealed an RE supertemporal macula on rhegmatogenous retinal detachment, most likely as a result of the horseshoe retinal tear visible around 10 o’clock in the above image (Fig1). There was mild nuclear sclerotic cataract in both eyes appropriate for her age.
Diagnosis and Discussion:
Diagnosis:
RE centre threatening macula-ON rhegmatogenous retinal detachment (RRD).
Discussion:
Recent developments in pars plana vitrectomy (PPV) protocol, particularly the use of small gauge instruments, have led to significant increase in the number of procedures done each year. One of the most commonly reported complications post vitrectomy is the accelerated formation of cataract. The exact cause for this accelerated development is unknown. More recent research has suggested a combination of increased oxygen tension in the eye, leading to oxidation of lens proteins, accumulation of cytokines in the anterior chamber and direct trauma from surgical instruments to the peripheral lens capsule. The use of gas has also been linked to an increased risk of cataract development.
For patients over the age of 50, it is most common to encounter nuclear sclerotic cataract, whereas those under 50 will more often develop posterior subcapsular changes. As a result of nuclear sclerotic change, as an optometrist you may see patients with rapidly increasing myopic shift. Research suggests that this progression occurs as a result of increasing refractive index of the lens material and a resulting increase in net spherical aberration of the lens. A small increase in lens thickness may also contribute to myopia development.
Treatment:
Visually significant cataract development and subsequent myopic shift are the most common side effects of PPV. Patients tend to present with similar symptoms to those with age-related cataract development. On top of this, some patients with rapid cataract progression may complain of diplopia or anisometropia. In those still working, these symptoms can present significant challenges with everyday tasks, such as driving or fine motor tasks. Cataract can also impede optometrists’ and ophthalmologists’ ability to accurately assess and monitor the retinal pathologies which initially required PPV treatment. As such research estimates that 50% of patients will have sequential cataract surgery within a year and 80% within 2 years.
Post-vitrectomy cataract surgery results in a number of unique challenges in addition to general cataract considerations. Patients undergoing vitrectomy should be counselled on the likelihood of cataract development and subsequent need for cataract surgery. When posterior segment pathology allows for it, combined phacovitrectomy should be considered. Research demonstrates visual outcomes are similar for phacovitrectomy when compared with sequential separate PPV and cataract surgery. There are benefits for patients including both reduced risk profile (due to single surgical procedure) and also financial benefits.
Intraocular lens consideration can also be challenging for these patients for a number of reasons. Firstly, it can be difficult to attain accurate biometry results for patients post vitrectomy, and particular attention must be paid to ensure the correct parameters are entered into optical biometers. For example, replacement of the vitreous with balanced salt solution or silicon oil induces refractive index changes, which must be taken into account when calculating IOL power.
Secondly, there is a clinically significant increase of in-the-bag dislocation in post-vitrectomy eyes. As such, the use of lenses requiring very accurate centration (such as a refractive multifocal IOL) is likely contraindicated. Furthermore, the presence of retinal pathology which may reduce contrast sensitivity means most presbyopia correcting lenses should be avoided. A monofocal IOL is most likely to maximise visual potential in these cases.
A third consideration is the refractive status of the fellow eye. If the patient is emmetropic in the fellow eye, the choice for the refractive aim for the IOL is straight-forward. However, if the patient is moderately myopic in their fellow eye, and it does not yet have significant cataract formation, the decision of what the refractive aim should be is more complicated. Significant anisometropia following surgery may necessitate the use of contact lenses to balance image size between the two eyes.
3-month follow up (post-vitrectomy and retinal detachment repair):
Unaided Visual Acuity:
RE: 6/30 LE: 6/12
Best Corrected Visual Acuity:
RE: -1.50 (6/9+) LE: +0.75 (6/12++)


Figure 2: Post-operative cataract development in RE and LE. The RE (on the left) demonstrates significantly more nuclear sclerosis and brunescence when compared with the LE.
At the 3-month follow up visit there was significant development of cataract in both eyes, with a significant myopic shift occurring in the right eye (Fig2). Careful examination of macular OCT scans showed no damage to the maculae of either eye, and the patient decided to have Extended Depth of Focus (EDoF) IOLs implanted in both eyes, with the goal of reducing dependence on glasses for near vision. Sequential cataract surgeries were completed successfully one month apart, with the visual outcomes detailed below.
Unaided Visual Acuity:
RE: 6/6 LE: 6/7.5
Binocular near visual acuity: n8 @ 40cm unaided
If your patient is experiencing sudden flashes, floaters or a shadow in their visual field, refer them to Queensland Eye and Retina Specialists for assessment and specialised treatment, if required.
Have any questions about patient eye care?