Cataracts 101
What is a Cataract?
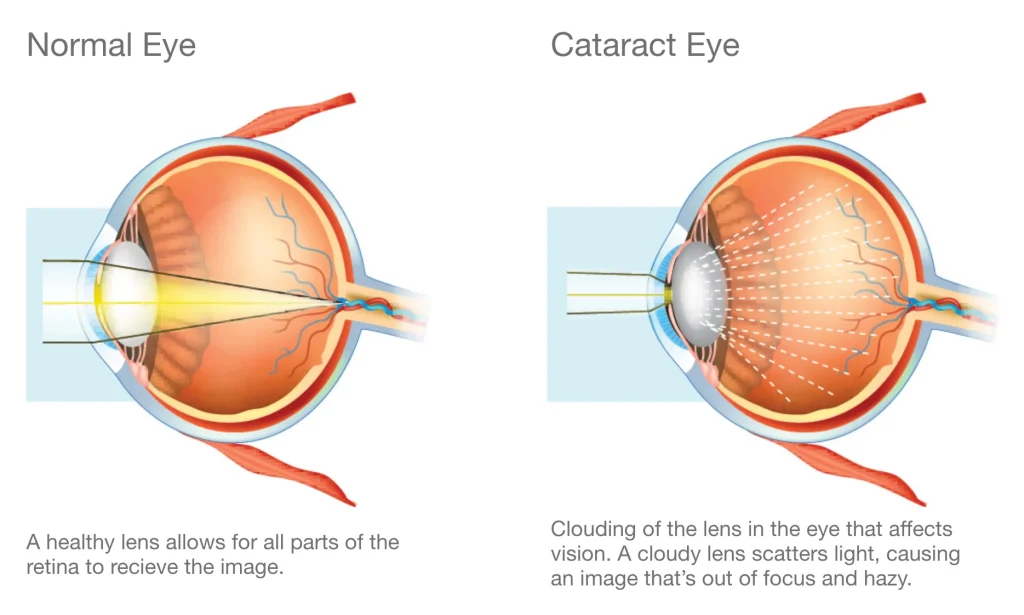
Cataracts happen as we age, when the natural lens of our eyes starts to degrade and cloud, turning a clear white or opaque colour. Cataracts affect half of all people over the age of 50 in Australia, and affect almost everyone by 80 years of age. Regular eye examination with your optometrist or ophthalmologist are crucial to diagnosis and treatment of cataracts.

Symptoms and Diagnosis
What Are the Signs of Cataracts?
When cataracts first appear, there’s a chance you won’t have any symptoms. But as cataracts develop over time, you may start to notice changes in your vision. Symptoms of cataracts include:
- Cloudy or blurry vision
- Light sensitivity
- Difficulty seeing at night
- Faded colours
- Double vision
- Glasses always seem dirty
- Halo around lights
How are Cataracts Diagnosed?
If you experience any of the above symptoms, it’s important to consult an optometrist for a comprehensive eye examination. For people aged 60 or older, you should get an eye exam every year. There are multiple tests used for cataract diagnosis:
- Visual Acuity Test: Also known as a vision test, this assesses your ability to see clearly at different distances both with and without glasses.
- Slit-Lamp Exam: A slit-lamp exam uses an instrument called a biomicroscope to complete a detailed examination of the different structures of the eye, such as the cornea, iris, and lens.
- Retinal Exam: This exam evaluates the back of the eye, specifically the retina and optic nerve. The eye specialist can examine the health of the retina through dilated pupils, identifying any signs of diseases such as diabetic retinopathy, macular degeneration, or retinal detachment.
- Tonometry: This test measures the intraocular pressure of the eye. Increased pressure in the eye can be a risk factor for glaucomaa

Causes and Types
What Are the Causes of Cataracts?
Ageing is the most common cause of cataracts as the proteins in the lens of your eye begin to break down after you reach age 40. However, there are other common causes of cataracts, such as:
- Family history of cataracts
- Serious eye injury or surgery
- Diabetes
- Obesity
- High myopic error
- Extended use of corticosteroid medication
- High alcohol consumption
- Smoking
- UV radiation
What are the Types of Cataracts?
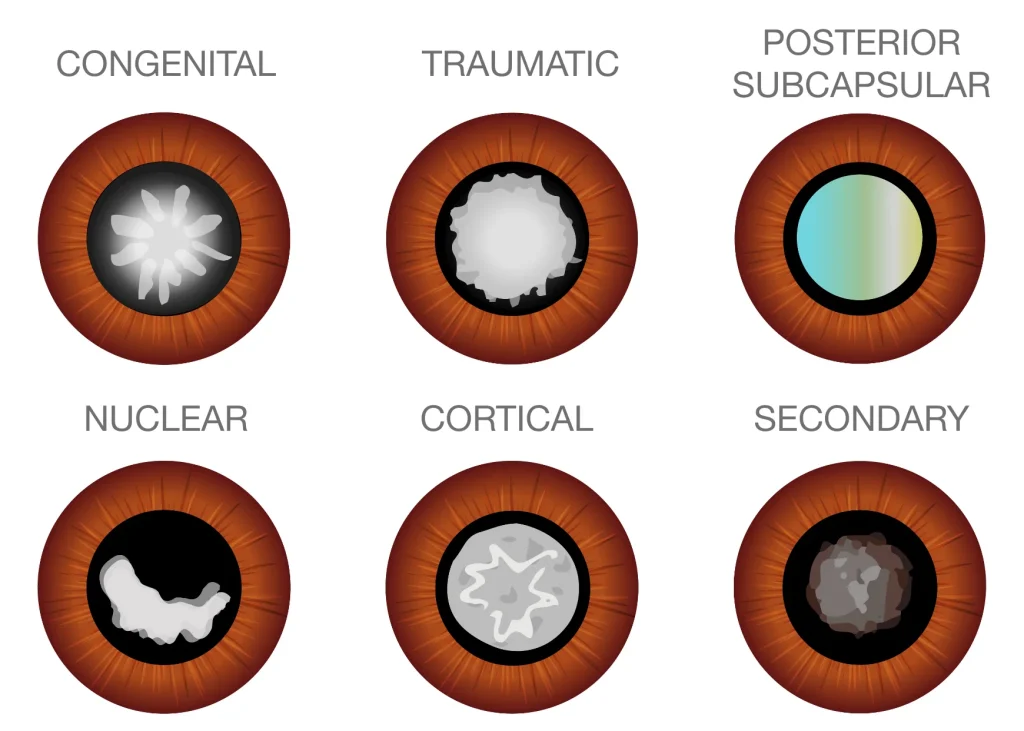
There are myriad different types of cataracts, all of which will result in some combination of the aforementioned symptoms. Treatment and diagnosis for the different types of cataracts is essentially the same. Regular eye examinations with your optometrist or ophthalmologist are essential in order to monitor progression of your cataract.
- Cortical cataracts develop in the outer portion of the lens, known as the cortex. They often present with a spoke-like pattern, extending from the periphery towards the centre.
- Nuclear cataracts affect the central or nuclear region of the lens and are characterised by yellowing and hardening of the central lens over time.
- Posterior subcapsular cataracts form at the back surface of the lens, just beneath the lens capsule, and are typically small opacities that can significantly impact vision.
- Posterior capsular opacification occurs for about 20% of patients after cataract surgery. This condition occurs as a result of leftover lens epithelial cells dividing and regrowing. They can cause blurred vision. Treatment involves a simple in-rooms laser procedure, known as a YAG laser capsulotomy. Once this has been treated, posterior capsular opacification cannot reoccur. People who have undergone eye surgery should remain vigilant and undergo regular follow-up examinations to monitor for potential secondary cataracts.
- Congenital cataracts are present at birth or develop during childhood. They can arise from genetic factors or prenatal influences, such as infections, trauma, or metabolic disorders affecting foetal development. Depending on their size and location, congenital cataracts may cause visual impairment and potentially lead to amblyopia (lazy eye) if not addressed promptly. Early diagnosis and intervention are key to managing congenital cataracts effectively.
Your Guide to Cataract Surgery Treatment
What Do I Need to Know About Cataract Surgery?
Cataract surgery is a highly effective treatment for restoring clear vision. In Australia, the procedure is widely accessible and is performed on more than 200,000 people each year. If cataracts are left untreated long enough, they will most cause blindness, so surgical treatment is usually necessary.
In most cases, cataract surgery does not require urgent treatment. The decision to undergo cataract surgery is one you and your surgeon should discuss together. Ask yourself these questions to determine whether you are ready to consult with an ophthalmologist:
- How severely is my sight affected?
- Can glasses still improve my vision?
- Is my vision impairment hindering me in completing my everyday tasks?
- What does my specialist recommend?
If you’re unsure on whether you should proceed with cataract surgery, contact the friendly team at Queensland Eye & Retina Specialists for evaluation and guidance.
What Should I Expect from Cataract Surgery?
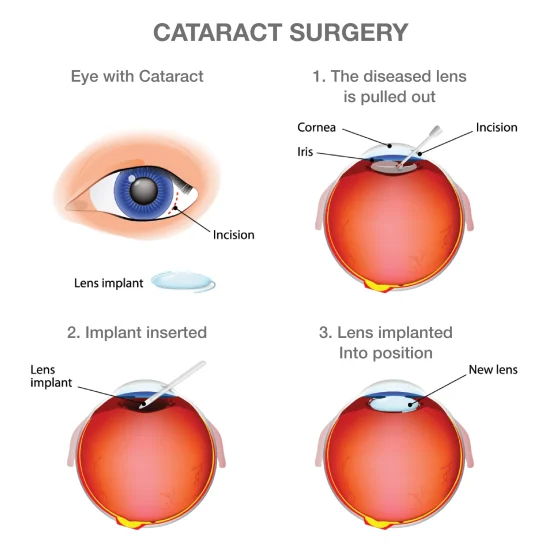
Cataract surgery is typically a 15 minute, relatively painless procedure that replaces the cloudy lens of your eye with an artificial one known as an intraocular lens (IOL). The doctor does this with an instrument known as a phacoemulsifier, that breaks up the cataractous lens and removes the pieces, before replacing it with the new IOL. Anaesthesia for cataract surgery most commonly involves intravenous twilight sedation and local anaesthetic eye drops. Unlike general anaesthesia, patients who have twilight sedation are still breathing for themselves. Hypnotic medications are used to ensure you do not remember any of the procedure.
What Happens After Cataract Surgery?
During the healing phase, your vision will be blurry, colours may seem brighter (as you are looking through a new and clear lens), and your eye will most likely feel itchy and uncomfortable – a normal part of the healing process. It’s important to avoid rubbing or pushing on your eye as it’s healing. Healing will typically be fully completed after four weeks, but the discomfort should settle a few days after the surgery.
You will be asked to wear a protective shield during the initial days and nights of recovery to avoid accidental rubbing of the eye. You will also be prescribed eye drops to prevent infection, control eye pressure, and reduce inflammation. Most patients will be required to take these drops for one month post-operatively.
Regular follow-up appointments with your doctor will be scheduled usually one day and then one month after surgery to monitor your recovery progress.
The team at Queensland Eye & Retina Specialists take a holistic approach, ensuring your eye health journey is informed and as smooth as possible. Contact us today for a consultation.